Actinic Keratoses (abbreviated, AK; precancerous)
Sun exposure can damage your skin, regardless of your skin color. Whether you have light, medium, or dark skin, the ultraviolet rays in sunlight harm and age your skin.
Light-skinned individuals are more likely to develop scaly, pink growths in areas of sun exposure. These are called Actinic Keratoses and are precancerous. Up to 10% of Actinic Keratoses may develop into skin cancer over many years.
When your dermatologist or trained medical professional examines your skin, they are searching for precancerous growths, Actinic Keratoses and Atypical Nevi (atypical “moles”), as well as non-spreading skin cancer like a Basal Cell Carcinoma. You are also checked to be certain that you do not have a more serious skin cancer, such as a Squamous Cell Carcinoma or a Melanoma.
Your dermatologist may use a lighted, magnifying device called a dermatoscope or dermascope to better evaluate your skin. Fortunately, Actinic Keratoses are easily treated. Skin cancer, if discovered early, can be successfully treated.

Dermatoscope
A special, lighted magnifying instrument is used to see “moles” more clearly.

Dermatoscope Exam

Actinic Keratoses
Multiple, rough, scaly papules on the right face—these growths are precancerous.

Actinic Keratoses
Scaly, pink papules are present on the left side of the face and neck.
These growths are precancerous. There is also a Squamous Cell Carcinoma (SCC) on the left mid-mandible developing from an Actinic Keratosis.

Actinic Keratoses
Multiple, scaly, pink papules on the left face; these lesions are precancerous.
Remember that you are personally unable to examine many areas of your own body, including your back, buttocks, back of your thighs, and back of your scalp. Your dermatologist or trained medical professional literally “has your back” in searching for skin cancer. A camera phone may enable you to look at some of these areas. Early detection of skin cancer can save your life and that of a family member or friend.
CAUSES OF ACTINIC KERATOSES
Many people get excessive sun exposure because of their jobs. For example, carpenters, fishermen, farmers, and gym teachers are often out in the sun for prolonged periods of time. People who frequently engage in outdoor sports are also at risk of excessive sun exposure. Sun damage, age changes, and Actinic Keratoses can be prevented by the use of sunscreens with a Sun Protection Factor (SPF of 30 or higher). Wearing protective clothing and staying in the shade also decreases your skin cancer risk.
Many people of all skin colors want a tanned, brown appearance. Tanning beds, tanning booths, and sun lamps can darken light skin, but usually this tan must be renewed every few weeks. These devices also age and damage your skin, causing precancerous growths and skin cancer after many years of repeated treatments. For this reason, medical professionals DO NOT recommend tanning beds, tanning booths, or sun lamps.
Medical professionals approve of a “spray tan,” which is generally a safe and effective way of darkening your skin. However, a spray tan will not protect your skin from sunlight unless sunscreen has been added to the spray tan solution. Sunscreens with an SPF of 30 or higher are still required to protect your skin from sun-induced damage, aging, and Actinic Keratoses.
Spray tans have an advantage over a “natural tan,” as your skin color can be lightened or darkened according to individual choice. Spray tans may be repeated every 7–10 days to maintain a tanned look.
RISK FACTORS FOR PRE-CANCERS, ACTINIC KERATOSES
Skin cancer occurs in all races, regardless of their skin color. It is more common in fair-skinned individuals. People who use tanning beds, tanning booths, or sun lamps are also at greater risk of developing skin cancer. See if you or your family have any of these risk factors:
Resources from the American Academy of Dermatology and the American Society for Dermatologic Surgery were consulted for this section.
DIAGNOSIS OF PRECANCEROUS ACTINIC KERATOSES
Actinic keratoses usually appear in areas of intense sunlight exposure (e.g. face, ears, nose, lips, scalp, neck, arms, and hands). Actinic Keratoses may vary in size and color. They usually have a pink, scaly appearance. If you rub sun-damaged areas, the skin will often feel rough to the touch.
Sometimes an Actinic Keratosis will grow abnormally and produce a growth that resembles a horn. This is called a “Cutaneous Horn” and is usually small. However, a cutaneous horn can rarely grow up to 25 cm (9.8 inches) in length. A cutaneous horn may have an underlying Actinic Keratosis or non-melanoma skin cancer (e.g. Basal Cell Carcinoma or Squamous Cell Carcinoma) at its base. The existence of Cutaneous Horns on humans may be the origin of reports of “horns” on mythical creatures like unicorns.

Cutaneous Horn, left post ear area
This has an Actinic Keratosis at its base.

Cutaneous Horn, left eyebrow area
This has a Squamous Cell Carcinoma at its base.
Actinic keratoses are usually diagnosed by visual exam by your dermatologist or trained medical professional. They may use a lighted, magnifying device called a dermatoscope or dermascope to better examine your skin. If an Actinic Keratosis does not have a classic appearance, a skin biopsy may be required to be certain that it is not a skin cancer.
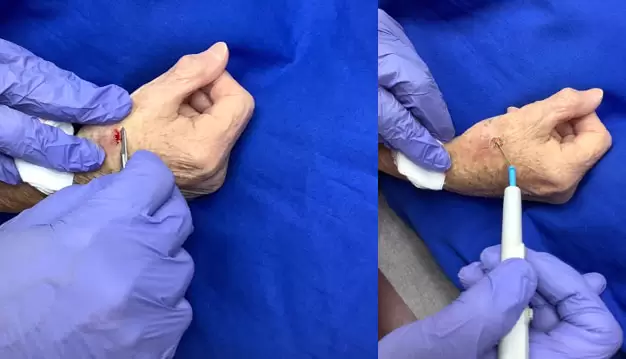
SKIN BIOPSY TECHNIQUE FOR A NON-HEALING GROWTH
LEFT A growth that does not heal or keeps recurring should be biopsied. After local anesthesia, a shave or scallop biopsy is performed using a scalpel with blade.
RIGHT The biopsy site is then “burned” (electrodessicated) with the probe from an electrosurgery device. The skin may also be curetted (scraped). The skin biopsy specimen and scrapings are sent to a pathology lab.
A dermatologist or trained medical professional can perform a skin biopsy during your office visit using local anesthesia. This procedure is fast, safe, and usually heals with minimal scarring. A small sample of your skin is sent to a pathology laboratory for processing and examination under a microscope by a pathologist. A pathology report on your skin biopsy is usually available within 7–14 days. If your growth is an Actinic Keratosis, no further treatment is usually necessary as the biopsy removes your Actinic Keratosis.
A skin biopsy is normally covered by Medicare, Medicaid, and insurance companies minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
SUMMARY OF TREATMENT OPTIONS FOR PRECANCERS / ACTINIC KERATOSES
Actinic keratoses are precancerous and should be evaluated during your visit to your doctor’s office. Your dermatologist or medical care professional can help you decide on the best treatment for your Actinic Keratoses:
(1) Cryosurgery for Actinic Keratoses
Cryosurgery is the most common treatment for Actinic Keratoses used by dermatologists and other medical professionals. It has a cure rate of over 90%. Actinic keratoses that do not respond to cryosurgery are usually re-treated with cryosurgery or biopsied to rule out skin cancer.

Cryosurgery Unit
Cryosurgery is frequently used to treat precancerous lesions (Actinic Keratoses)

Cryosurgery Treatment
Treatment of Actinic Keratoses with cryosurgery
Cryosurgery treatment consists of the spray application of liquid nitrogen to the Actinic Keratoses sites. Liquid nitrogen is very cold and freezes the treatment area. The treatment area will immediately become frozen and turn white. The white color fades over a few minutes as the area unfreezes. The site then becomes pink and slightly swollen for several days, followed by crusting. For the best cosmetic results, do not disturb this crust and allow the treatment site to heal over the next 3–4 weeks. Occasionally, small blisters will form at the treatment sites. These can be opened with a sewing needle that has been cleansed first with rubbing alcohol. Areas with the most sun damage take longer to heal.
Cryosurgery is normally covered by Medicare, Medicaid, and insurance companies, minus any deductible or co-payment required by your insurer.
If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
(2) Chemical Treatment for Actinic Keratoses
A Chemical Treatment for Actinic Keratoses is also regularly used by dermatologists and other health professionals. 5-Fluorouracil 5% cream is often prescribed to treat Actinic Keratoses. The estimated cure rate is 86% or higher. The anti-cancer cream, ointment, or solution is applied according to directions once or twice a day for 2-4 weeks or more while avoiding the eye areas.

5-Fluorouracil 5% Cream is commonly used to treat precancerous areas (Actinic Keratoses). The usual treatment course is once or twice a day for 2-4 weeks while avoiding the eye areas.
This cream is sometimes used after skin cancer treatment in order to prevent a skin cancer recurrence. It is occasionally employed to treat Superficial Basal Cell Carcinoma but its use is NOT usually recommended for other skin cancers (e.g. non-superficial basal cell carcinoma, squamous cell carcinoma, and melanoma). Topical treatment may not reach skin cancer cells that are deep in the skin. Consequently, the surface of the skin cancer may heal while allowing the deeper part of the skin cancer to enlarge and spread (metastasize). 5-Fluorouracil 5% cream has a 90% or higher success rate with Superficial Basal Cell Carcinoma.
Areas treated with 5-Fluorouracil 5% cream will become red, swollen, tender, and may ooze during and after treatment. The areas crust over and will take 2-4 weeks to heal AFTER completing your 2–4-week course of anti-cancer cream therapy. Areas with the most sun damage take longer to heal.
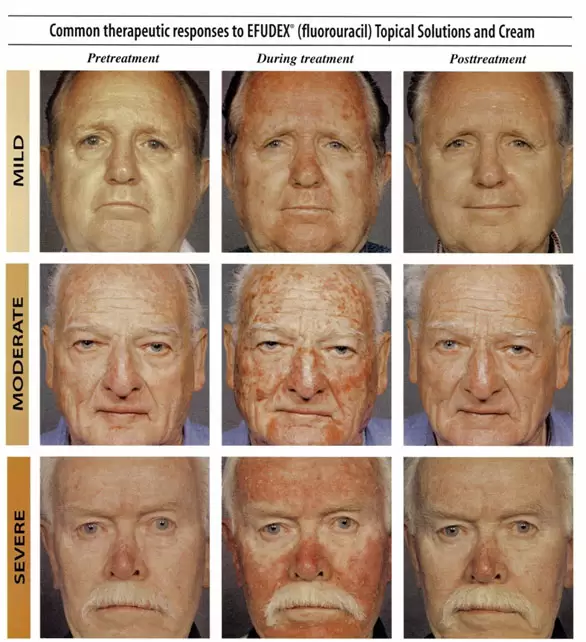
COLUMN 1 is a Before picture of Actinic Keratoses, Mild, Moderate, and Severe.
COLUMN 2 is During 5-Flurouracil treatment; note the redness and crusting;
COLUMN 3 shows skin healing about one month after completing 5-Fluorouracil treatment

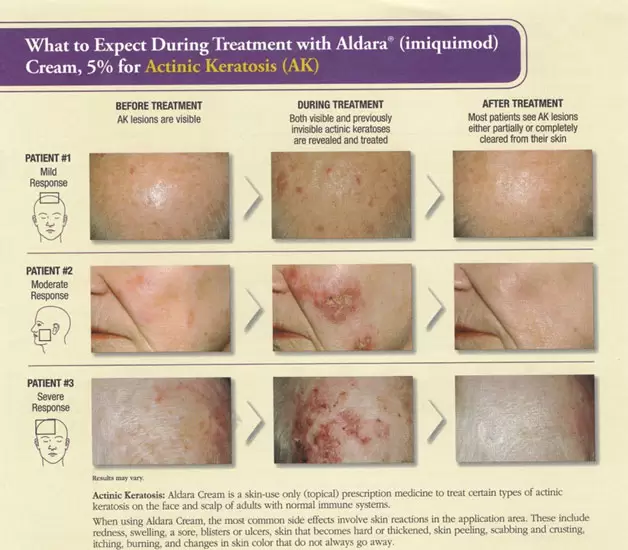
Imiquimod 5% cream is sometimes used to treat precancerous skin lesions (Actinic Keratoses). The cream works by stimulating the immune system.
Imiquimod 5% cream is sometimes used to treat Actinic Keratoses. The cream works by stimulating the immune system. The cream usually comes in packets and a small amount is applied to the affected areas while avoiding the eyes. Imiquimod 5% cream is used 2 or 3 days a week for 16 weeks or longer for the treatment of Actinic Keratoses. The complete clearance rate is 57%, and the partial clearance rate is 72%.
This cream is sometimes used after skin cancer treatment to prevent skin cancer recurrence. It is also rarely used to treat Superficial Basal Cell Carcinoma, but its use for other types of skin cancer (e.g., Basal Cell Carcinoma, Squamous Cell Carcinoma, and Melanoma) is NOT usually recommended. Topical treatment may not reach skin cancer cells that are deeper in the skin. Consequently, the surface of the skin cancer may heal while allowing the deeper part of the skin cancer to enlarge and spread (metastasize).
Areas treated with imiquimod 5% cream will become red, swollen, tender, and may ooze during and after treatment. The areas then crust over and will take 2–4 weeks to heal AFTER completing your 16-week course of therapy. Areas with the most sun damage take longer to heal.

Tirbanibulin 1% ointment (KlisyriTM) is a new alternative treatment for precancerous skin growths (Actinic Keratoses). Tirbanibulin 1% ointment is a microtubule inhibitor that stops the growth and spread of skin cancer. It is usually applied once a day for five days while avoiding the eye areas. Areas treated with Tirbanibulin 1% ointment may become red, swollen, tender, and ooze during and after treatment. The treatment sites heal within 2–4 weeks. Areas with the most sun damage take longer to heal.
Tirbanibulin 1% ointment has a 54% complete clearance rate for Actinic Keratoses. The effectiveness of this cream for non-melanoma skin cancer (e.g. Basal Cell Carcinoma and Squamous Cell Carcinoma) is unknown at this time. Tirbanibulin 1% ointment is best obtained by sending your anti-cancer prescription to a specialty pharmacy through your doctor’s office
TO SUMMARIZE, areas treated with a traditional anti-cancer cream, ointment, or solution will become red, swollen, tender, and may ooze during and after treatment. The treated areas often crust over. It will take 2-4 weeks for your skin to heal AFTER completing your course with anti-cancer creams, ointments, or solution like 5-Fluorouracil 5% cream or imiquimod cream 5%. Tirbanibulin 1% ointment also takes 2-4 weeks to heal AFTER completion of a five-day treatment course. Areas with the most sun damage take longer to heal. Topical Chemical Treatment may have to be repeated several times a year to maintain clearance of Actinic Keratoses.
Actinic keratoses that do not respond to chemical treatment are usually treated with cryosurgery [See (1) above] or are biopsied to rule out skin cancer.
Medicare, Medicaid, and most insurance companies will cover the cost of your doctor’s visit for treatment of Actinic Keratoses and a routine skin evaluation minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
Insurance companies will sometimes not cover the cost or will delay payment for a prescription anti-cancer cream, gel, or ointment. This problem can be avoided by sending your prescription to a specialty pharmacy through your doctor’s office.
(3) Blue or Red Light Therapy (also known as Photodynamic Therapy or PDT)
Blue or Red Light Therapy is used when there are more extensive actinic keratoses on the face, neck, trunk, and extremities. This therapy is also called photodynamic Therapy or PDT. Blue or Red Light Treatments leave the skin smooth, “like a baby’s skin”. Red Light Therapy may go deeper into the skin than Blue Light Therapy. For this reason, Actinic Keratoses treated with Red Light Therapy may take slightly longer to heal than with Blue Light Therapy.
Blue or Red Light Therapy consists of the application of a special solution or gel to the treatment areas and surrounding skin at your doctor’s office or clinic. The solution or gel gets into the “nooks and crannies” of your skin and makes your skin sensitive to blue and red light.
After a waiting time of 1 hour (face and scalp), 2 hours (chest and arms), and 3 hours (legs and back), a Blue Light Treatment is administered from a light stand for 10 to 16.5 minutes or longer. For Red Light Therapy, the light source is smaller and usually requires two 10-minute treatments for a treatment area. A larger light source for Red Light Therapy is pending approval.
After the Blue or Red Light treatment, your skin becomes red, slightly swollen, and tender. You should avoid sunlight and protect yourself from the sun for the next 24–48 hours, as you may have become sun-sensitive. Your skin will usually heal within a few weeks, leaving behind improved, smoother skin. There is usually an 80% or higher cure rate. Non-responsive or recurrent growths are usually treated with cryosurgery or biopsies to rule out skin cancer.
Repeat Blue or Red Light Therapy may be required 2-4 times per year, depending on how well your Actinic Keratoses and actinic damage respond to therapy.
Medicare, Medicaid, and Insurance plans usually cover Blue or Red Light Treatment for Actinic Keratoses minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
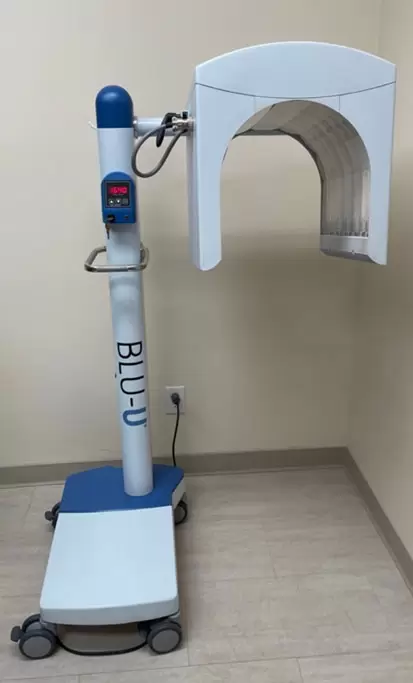
Blue Light Unit
Blue and Red Light treatments are used to treat sun-damaged skin and precancerous lesions (Actinic Keratoses)

Blue Light Treatment
Patient receiving Blue Light Treatment to the Arms for Actinic Keratoses

A patient receiving Blue Light Treatment for Actinic Keratoses and two Squamous Cell Carcinomas on his scalp
Blue Light Therapy (Photodynamic Therapy, or PDT) for precancerous, Actinic Keratoses

COLUMN 1 shows precancer areas (Actinic keratoses) Before Blue Light Treatment.
COLUMN 2 shows treatment sites 48 hours later; Note the redness and scaling.
COLUMN 3 shows the treatment sites after one week, which have mostly cleared up.
COLUMN 4 after 4 weeks shows clearer, smoother skin.
(4) Electrodessication and Curettage for Actinic Keratoses
A small precancerous growth can be removed under local anesthesia by “burning and scraping”. The growth is treated with electrodessication (“burning”) with the probe of an electrosurgery device to stop bleeding. This is followed by “scraping” with a curette (curettage) to remove superficial skin damage. This may be repeated several times. The cure rate is over 95% for Actinic Keratoses.
If your growth is suspicious for skin cancer, a sample of your curetted skin is sent to a pathology laboratory for processing and examination under a microscope by a pathologist. A pathology report is usually available within 7–14 days. Your dermatologist or trained medical professional will discuss your pathology report with you on your next doctor’s visit. If a skin cancer diagnosis is reported on your pathology report, your treatment options will be discussed with you at the time of your next doctor’s visit.
This treatment is usually covered by Medicare, Medicaid, and insurance companies minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.

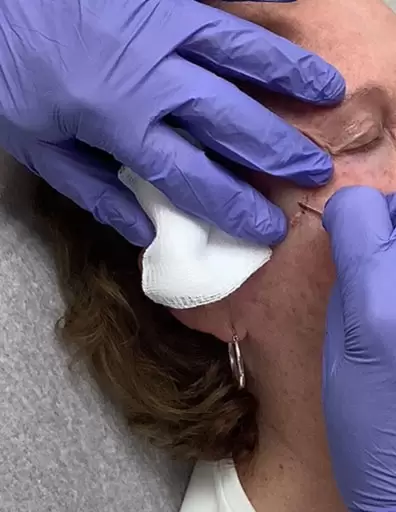
TREATMENT OF ACTINIC KERATOSES WITH ELECTRODESSICATION AND CURETTAGE
A non-healing growth or recurrent Actinic Keratosis should be biopsied and treated.
LEFT After the area is numbed up with local anesthesia, the area is biopsied with a scalpel. The area is then cauterized with the probe of an electrosurgery device, as shown here.
RIGHT - The area is then curetted (scraped) to remove any residual growth. The biopsy and scrapings are sent to a pathology lab.
(5) Laser Resurfacing for Actinic Keratoses
Extensive Actinic Keratoses can be treated with an ablative laser, which removes the top layers of the skin. This is also known as laser resurfacing. A Secret Pro™, Mixto™ laser, Fraxel™ laser, Ultrapulse™, and Erbium-YAG laser are examples of ablative lasers. This type of laser is also employed to tighten your skin, remove unwanted growths, even out your skin color, and smooth surface irregularities. Treatment time will depend on the number of areas that are treated. Ablative lasers have an estimated cure rate of over 90% for Actinic Keratoses.

BEFORE / AFTER 2 Weeks after laser resurfacing
Laser resurfacing can remove sun-damaged skin and Actinic Keratoses. It also tightens the skin and removes wrinkles.
[Photos courtesy of Dr. Andrew A. Hendricks.]

BEFORE / AFTER 2 Weeks after laser resurfacing
[Photos courtesy of Dr. Andrew A. Hendricks]


A Mixto™ is an ablative laser that uses carbon dioxide (CO2) to remove skin damage. Other carbon dioxide lasers include Ultrapulse™, Fraxel™, and Secret Pro™. These lasers not only tighten and smooth the skin but also remove wrinkles, age lines, and brown spots.
Thulium™ and ErbiumYAG™ use different energy methods but achieve similar results.
Medicare, Medicaid, and insurance companies may cover Laser Treatment for 15 or fewer Actinic Keratoses. Your doctor can advise you further on treatment costs, which depend on the extent and type of your laser treatment.
(6) Chemical Peels for Actinic Keratoses
Alternately, a moderate-to-deep Chemical Peel can be used to improve the skin’s appearance as well as eradicate Actinic Keratoses. A Chemical Peel offers a convenient way to treat Actinic Keratoses on your face and other skin areas. Treatment time is 15–30 minutes or longer, depending on the type of chemical peel and the treatment area. Areas treated with a Chemical Peel become red, swollen, tender, and ooze clear fluid. The cure rate will depend on the type and depth of the chemical peel.
Medicare, Medicaid, and insurance companies may cover Chemical Peel Treatment for 15 or fewer Actinic Keratoses. Your doctor can advise you further on treatment costs, which depend on your type of chemical peel and the treatment size.