Melanoma and Pre-Melanoma
Melanoma is considered the most dangerous of ALL types of cancer due to its easy ability to spread into the bloodstream to other areas of the body (i.e., metastasize). However, if Melanoma is diagnosed early, the cure rate can be 100%.
Melanoma arises in the pigment-producing cells of your skin, called melanocytes. Melanocytes give your skin its color. Melanocytes are located in the base layer of the epidermis. The epidermis is the outermost layer of your skin and is just the thickness of a piece of paper.
Over 50% of the time, Melanoma develops as a new growth, not in an existing “mole.” It is important to have your skin checked regularly by a family member, a dermatologist, or a trained medical professional.
You should realize that you are unable to see many areas of your body, including your back, buttocks, back of your thighs, back of your neck, and back of your scalp. Your dermatologist or trained medical professional literally “has your back” in searching for skin cancer. They may use a lighted, magnifying device called a dermatoscope or dermascope to better evaluate your skin. Fortunately, most Melanomas are discovered early and can be successfully treated.
A camera phone may assist you in your self-inspection of these areas. Remember, early detection of a melanoma can save your life and that of a family member or friend. Over 100,000 people develop melanoma in the United States each year and 10,000 die from it.
WHAT “MOLES” SHOULD BE CHECKED?
. Any mole that is growing rapidly or changing in shape or color
. Any mole that bleeds or oozes
. Any growth that is itching, painful, or bleeding
. A streak (usually brown or black) that appears in a fingernail or toenail
. Any non-healing “sore” or growth
Resources from the American Academy of Dermatology and the American Society for Dermatologic Surgery were consulted for this section.

Dermatoscope
A special, lighted magnifying instrument is used to see “moles” more clearly

Dermatoscope Exam

Melanoma in situ
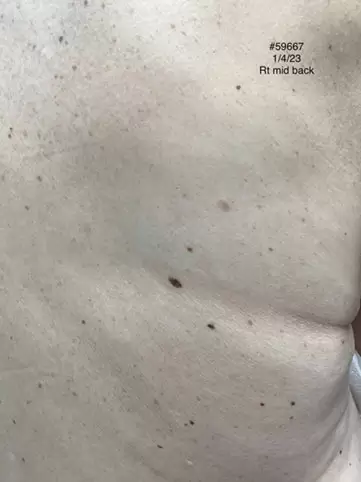
Right mid-back

Melanoma in situ
Right cheek
Melanoma in situ is 100% curable by early diagnosis and wide surgical excision. For this reason, it is important to make an early diagnosis of Melanoma in situ.

Melanoma in situ, right, mid-lateral back
Surgical removal is required

Moderate-Severe Atypical (Dysplastic) Nevus, right mid-back
A Moderate-Severe or Severe Atypical (Dysplastic) nevus requires surgical Removal as it may change into melanoma.
RISK FACTORS
Many Melanomas can be prevented by protecting your skin from the sun. Sunscreens with a Sun Protection Factor (SPF) of 30 or higher are very effective in blocking the harmful ultraviolet rays of the sun. Protecting yourself from the sun and wearing sun-protective clothing also helps to prevent Melanoma as well as pre-cancerous growths (Actinic Keratoses) and non-melanoma skin cancer (e.g., Basal Cell Carcinoma and Squamous Cell Carcinoma).
If you have a family history of Melanoma, your risk of developing it is increased. A family history of non-melanoma skin cancer also puts you at greater risk of Melanoma.
Risk factors for developing Melanoma are similar to those of pre-cancerous growths like Actinic Keratoses and cancerous growths like Basal Cell Carcinoma and Squamous Cell Carcinoma. See if you or your family have any of these Risk Factors:
Resources from the American Academy of Dermatology and the American Society for Dermatologic Surgery were consulted for this section.
DIAGNOSIS
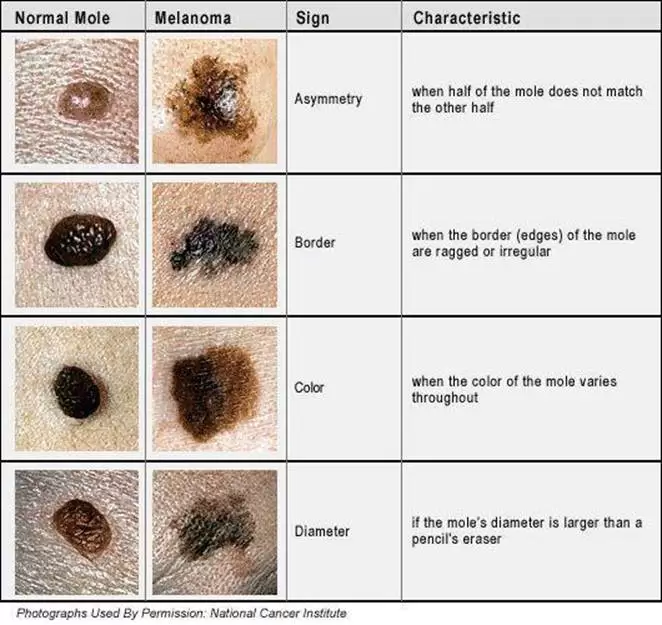
A Melanoma may appear on the skin with no precursor growth over 50% of the time. People are reminded to “Remember their ABCs” for diagnosing an Atypical “Mole” (known medically as an Atypical Nevus or Dysplastic Nevus) and for diagnosing Melanoma.
An Atypical / Dysplastic nevus is considered a Pre-Melanoma. Some Pre-Melanoma growths will change into melanoma over a period of time.
If you notice the following ABCDEF changes in growth, consult your dermatologist or trained medical professional.
A is for an Asymmetrical appearance
B is for an irregular Border
C is for an atypical brown, tan, black Color or Multi-color. In some instances, the atypical growth may appear pink or have no color. This is called an Amelanotic Melanoma. This is a rare type of Melanoma that is often diagnosed late due to the lack of color changes.
D is for the Diameter or size of the lesion. Although most Melanomas are 0.6 cm (about 1/3 inch) or more in Diameter when they are diagnosed, some melanomas may be only the size of a pencil mark.
E is for Evolving. A growth that is changing in size, shape, color, or elevation should be biopsied. Also, if the growth is itching, oozing, bleeding, or crusting, it should be biopsied.
F is for Funny-Looking. This is included in the ABCs of melanoma detection, as it helps guide whether to do a skin biopsy. If all the skin lesions appear "funny-looking,” then this pattern may be normal for an individual. But if a growth does not look like it belongs with other skin growths, it should be biopsied. This is known as the “ugly duckling sign”.
Melanoma can occur in all people, regardless of their skin color. People of color develop melanoma in areas where they get little sun exposure. 60–75% of all melanomas in people of color are found on their hands, soles of the feet, and nail areas.
**The Bottom Line is that All suspicious growths should be biopsied.**
Your dermatologist or trained medical professional will carefully examine your skin. They may use a lighted, magnifying device called a dermatoscope or dermascope to better see your skin. Remember, you cannot physically see the back of your head, the back of your neck, your back, your buttocks or your posterior thighs. Your dermatologist or trained medical professional literally “has your back” in searching for skin cancer. A camera phone may also allow you to see your back.
Any growth that looks suspicious should be biopsied. This involves removing a sample of your skin under local anesthesia. A skin biopsy is quick, safe, and usually heals with minimal scarring.
To diagnose a Pre-Melanoma or Melanoma, your dermatologist or trained medical professional can perform a skin biopsy under local anesthesia at the time of your office visit. This is the only way to confirm the diagnosis of skin cancer. A skin biopsy procedure is fast, safe, and usually heals with minimal scarring.
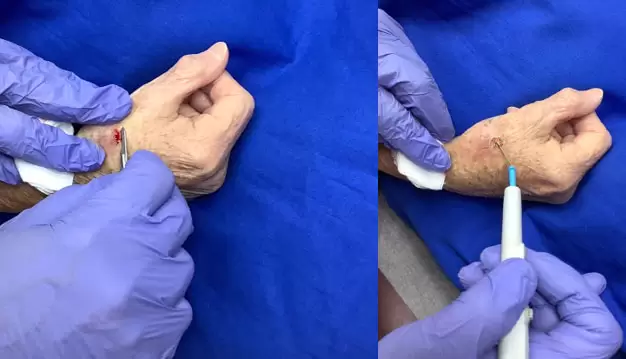
SKIN BIOPSY TECHNIQUE FOR A SUSPICIOUS OR NON-HEALING GROWTH
LEFT A growth that does not heal or keeps recurring should be biopsied. After local anesthesia, a shave or scallop biopsy is performed using a scalpel with blade.
RIGHT The biopsy site is then “burned” (electrodessicated) with the probe from an electrosurgery device. The skin may also be curetted (scraped). The skin biopsy specimen and scrapings are sent to a pathology lab.
Your skin biopsy specimen is sent to a pathology laboratory for processing and examination under a microscope by a pathologist. A pathology report is usually available within 7–14 days. Your dermatologist or trained medical professional will discuss your pathology report with you at the time of your next doctor’s visit. If a skin cancer diagnosis is found on your pathology report, treatment options will be discussed with you. Remember, if a Pre-Melanoma or Melanoma in situ is diagnosed early, they can be cured 100% of the time.

Mildly Dysplastic Nevus
A skin biopsy shows a mildly Atypical Nevus. No excision is required.
Moderately Atypical (Dysplastic) Nevus on skin biopsy
No excision is required

Dysplastic Compound Nevus with Moderate Atypia on skin biopsy.
A Moderately Dysplastic (Atypical) Nevus does not usually require excision.

Moderate-Severe or Severely Atypical Nevus
require surgical removal (excision).
A skin biopsy is covered by Medicare, Medicaid, and other insurance companies, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
TREATMENT OPTIONS FOR PRE-MELANOMA AND MELANOMA
Treatment for Pre-Melanoma or Melanoma depends on its size, depth, and location. If the Pre-Melanoma (known as an Atypical Nevus or Dysplastic Nevus) is “severely atypical,” it should be excised with a 0.4 cm (about a 0.2 inch) margin. Mild or moderate atypical/dysplastic nevi usually require no further treatment.
If your Melanoma has NOT penetrated below the skin surface, it is known as “Melanoma in Situ” or “STAGE 0”. These tumors are usually excised with up to a 1.0 cm margin around the Melanoma in Situ with a 100% cure rate.
Melanoma that has penetrated through the top layer of skin, known as the epidermis, into the underlying dermis is considered “STAGE I." These lesions carry a good prognosis with a wide surgical excision with 1 cm or larger margins.
The majority of Melanomas are treated by simple excision with no need for further cancer treatment. Mohs surgery is currently being evaluated for Melanoma treatment.
If the Melanoma has penetrated through the epidermis more than 0.8 mm (Breslow’s level) into the dermis, the tumor is classified as "STAGE II”. At this point, patients are usually referred to a Melanoma Clinic for a sentinel lymph node biopsy and a wide surgical excision.

TREATMENT OF MELANOMA, PRE-MELANOMA, AND NON-MELANOMA SKIN CANCER (Basal Cell Carcinoma and Squamous Cell Carcinoma) with EXCISIONAL SURGERY
Skin Cancer should be excised (cut out) in a doctor’s office under local anesthesia.
PHOTO 1: First, a drawing is made around the skin cancer. The size of the drawing around the skin cancer is usually 4–10 mm (0.17 to 0.4 inches), which assures that the skin cancer will be completely excised.
PHOTO 2: The marked area is then excised (cut out) using a scalp with a sharp blade.
PHOTO 3: Any bleeding is cauterized (burned) with the probe of an electrosurgery device.
PHOTO 4: The final step is to tie the skin together with sutures (stitches)
If the lesion extends into the sentinel lymph node, it is reclassified as “STAGE III”. If the tumor spreads beyond the lymph nodes to other parts of the body, it is classified as “STAGE IV”. Each of these stages carries a less favorable prognosis.
Melanoma treatment is covered by Medicare, Medicaid, and other insurance companies, minus any deductible or co-payment required by your insurance carrier. If you have a second insurance policy (“secondary insurance”), this will cover up to 20% of your total billing charges.
TREATMENT FOR ADVANCED MELANOMA
When Melanoma spreads into the lymph nodes (STAGE III) or to more distant parts of the body (STAGE IV), it is considered advanced, and additional treatments are required. Due to recent breakthroughs in treatment, the 5-year survival rate of patients with advanced Melanoma is now about 50%.
Treatments for advanced Melanoma are usually coordinated by an oncologist (cancer specialist) at a cancer facility. These treatments are covered by Medicare, Medicaid, and other insurance carriers, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover the co-payment.
IMMUNOTHERAPY FOR ADVANCED MELANOMA
Medications that boost the immune system are known as immunotherapy drugs. These include:
Pembrolizumab (Keytruda™) [infused intravenously for STAGE IIB, and STAGE IIC after melanoma surgery to prevent tumor progression; this therapy has been very promising].
Pembrolizumab (Keytruda™) [infused intravenously for STAGE III and STAGE IV patients]
Pembrolizumab (Keytruda™) and Sotigalimab (humanized IgG1 monoclonal antibody) [infused intravenously for STAGE IV patients]
Ipilimumab (Yervoy™) [infused intravenously for STAGE III and IV patients]
Nivolumab (Opdivo™) [infused intravenously for STAGE III and STAGE IV patients]
Nivolumab (Opdivo™) and Relatlimab are infused intravenously for STAGE IV patients. This protocol is preferred by some oncologists.
Nivolumab (Opdivo™ and ipilimumab (Yervoy™) (combination [infused intravenously for STAGE IV patients]) have shown promising results.
Talimogene laherparepvec [T-VEC] (Imlygic™) injected into the tumor for STAGE III and STAGE IV patients
MELANOMA VACCINE
A recent study using Moderna, Inc.’s personalized cancer vaccine with Keytruda™) immunotherapy showed 79% of high-risk melanoma patients were alive and cancer-free at 18 months, compared to 62% receiving immunotherapy alone.
Historically, earlier immunotherapies were the first FDA-approved drugs, but they are not as beneficial as the newer therapies listed above.
Interferon alfa-2b (Intron A™) [infused intravenously or injected subcutaneously or intramuscularly for high-risk STAGE II and STAGE III patients]
Pegylated interferon alfa-2b (Pegintron™), Interleukin-2 (Proleukin™/ aldesleukin) [infused intravenously for STAGE IV patients.]
TARGETED DRUG THERAPY FOR ADVANCED MELANOMA
New targeted therapies for advanced Melanoma are all taken by mouth.
They target a defective, cancer-producing version of the gene called BRAF.
About half of Melanoma patients have this mutant gene. Only patients with the mutant gene will benefit from Targeted Drug Therapy.
Targeted oral drug medications for Melanoma include:
Nivolumab (Opdivo™) and ipilimumab (Yervoy™) intravenously, followed by the oral drugs, dabrafenib (Tafinlar™) and trametinib (Mekinist™) This combination is superior to other drug combinations for patients with advanced BRAF V600 metastatic melanoma. The results have been very encouraging.
Dabrafenib (Tafinlar™), oral medication
Trametinib (Mekinist™), oral medication
Combination of Dabrafenib (Tafinlar™) and Trametinib (Mekinist™) for STAGE III and IV patients
Vemurafenib (Zelboraf™) and Cobimetinib-(Cotellic™) combination for STAGE IV patients
Encorafenic (Braftovi™) and binimetinib (Mektovi™) combination for STAGE IV patients
Atezolizumab (Tecentriq™)-cobimetinib (Cotellic™)-vemurafenib (Zelboraf™), combination for patients with BRAF V600 mutation-positive melanoma
These advanced Melanoma treatments are covered by Medicare, Medicaid, and other insurance carriers, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
RADIATION THERAPY FOR ADVANCED MELANOMA
Early studies show that experimental radiation therapy with some medications may be beneficial.
Resources from the American Academy of Dermatology and the American Society for Dermatologic Surgery were used for this section.