Squamous Cell Carcinoma (abbreviated, SCC)
Squamous Cell Carcinomas (SCC) is a common type of skin cancer that typically appears in sun-exposed areas of your body. SCCs are caused by the ultraviolet rays in sunlight. About one million people develop SCCs in the United States every year. This is about the same number of patients who develop traditional cancers each year in the United States (e.g., breast cancer, colon cancer, prostate cancer, and more).
When your dermatologist or trained health professional examines your skin, they are searching for precancerous growths, Actinic Keratoses, Atypical Nevi (atypical “moles”), and non-spreading skin cancer like Basal Cell Carcinoma. They are also checking to be certain that you don’t have a more serious skin cancer, such as a Squamous Cell Carcinoma or a Melanoma.
Your dermatologist or trained medical professional may use a lighted magnifying device called a dermatoscope to better examine your skin.
Fortunately, most precancerous growths, atypical "moles," and skin cancers are discovered early and can be successfully treated.
Remember, you are physically unable to examine many areas of your own body, including your back, buttocks, back of your thighs, back of your neck, and back of your scalp. Your dermatologist or trained medical professional literally “has your back” in searching for skin cancer. A phone camera can sometimes help you examine these areas. Early detection of skin cancer can save your life and that of a family member or friend.
Squamous Cell Carcinoma often develops from an untreated precancerous growth called an Actinic Keratosis. SCCs may also appear elsewhere on the body including inside the mouth, on the lips, or on the genitals. These same areas are at high risk of the SCC spreading locally or internally (metastasizing). Mohs surgery is the preferred treatment in these areas.
Squamous Cell Carcinomas are more aggressive than Basal Cell Carcinomas. A SCC usually develops in sun-exposed on the face, neck, trunk, and extremities. As there is a risk of spreading locally or into the blood stream (metastasizing), all SCCs should be treated and monitored.
SCC lesions may have many different appearances. Usually, they appear as a red bump that may be scaly or crusted over. An SCC growth may be non-healing, itching, or bleeding. It may appear to heal for a few weeks but then recur at the same site. Generally, any suspicious area should be checked by your dermatologist or a trained medical professional.

Dermatoscope
A special, lighted magnifying instrument is used to see “moles” more clearly

Dermatoscope Exam

Squamous Cell Carcinoma
left lateral cheek

Squamous Cell Carcinoma
right lateral neck

Squamous Cell Carcinoma left lower lip
This is a high-risk growth that can invade locally and spread into the bloodstream (metastasize)
RISK FACTORS FOR SQUAMOUS CELL CARCINOMA
Squamous Cell Carcinoma occurs in all races, regardless of their skin color. It is more common in fair-skinned individuals. People who use tanning beds, tanning booths, or sun lamps are also at greater risk of developing skin cancer. See if you or your family have any of these Risk Factors:
Resources from the American Academy of Dermatology and the American Society for Dermatologic Surgery were consulted for this section.
DIAGNOSIS OF SQUAMOUS CELL CARCINOMA
To diagnose a Squamous Cell Cell Carcinoma (SCC), your dermatologist or trained medical professional performs a skin biopsy under local anesthesia at the time of your office visit. This is the only way to confirm the diagnosis of skin cancer. A skin biopsy procedure is fast, safe, and usually heals with minimal scarring.
If you have a suspicious growth, a small sample of your skin is surgically removed (i.e., biopsied) under local anesthesia. This specimen is sent to a pathology laboratory for processing and examination under a microscope by a pathologist. A pathology report is usually available within 7–14 days.
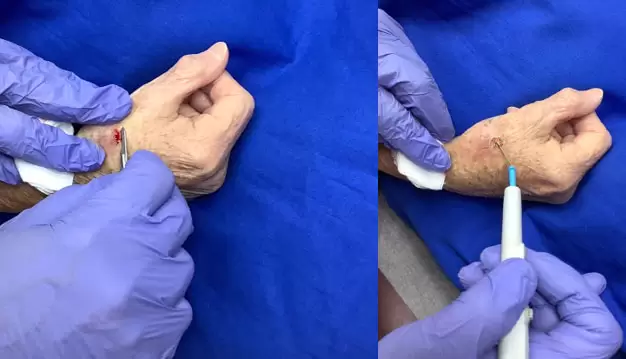
SKIN BIOPSY TECHNIQUE FOR A NON-HEALING GROWTH
LEFT A growth that does not heal, keeps recurring, or looks suspicious should be biopsied. After local anesthesia, a shave or scallop biopsy is performed using a scalpel with blade.
RIGHT The biopsy site is then “burned” (electrodessicated) with the probe from an electrosurgery device. The skin may also be curetted (scraped). The skin biopsy specimen and scrapings are sent to a pathology lab.
Your dermatologist or medical care professional will discuss your pathology report with you at the time of your next doctor’s visit. If a skin cancer diagnosis is found on your pathology report, treatment options will be discussed with you.
A skin biopsy is normally covered by Medicare, Medicaid, and insurance companies, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this usually covers your co-payment.
TREATMENT OPTIONS FOR SQUAMOUS CELL CARCINOMA
Treatment for Squamous Cell Carcinoma (SCC) depends on the location, size, type, and age of the patient. Squamous Cell Carcinoma, like Basal Cell Carcinoma, can cause disfigurement due to local invasion and destruction of underlying skin structures. SCC also has the potential to spread locally or into your blood stream (metastasize). It is important that you receive appropriate treatment for your SCC. Your dermatologist or medical professional can help you decide on the best treatment.
Many conflicting factors are considered when making a treatment recommendation for skin cancer. If the base of the SCC is less than 1.0 cm (0.4 inches) in size, it is considered low-risk. If the lesion base is over 1.0 cm (0.4 inches) in size, it is high-risk. If the SCC is located near an eye, ear, nose, mouth, or temple area, it is considered very high risk. If the SCC is poorly differentiated, there is a greater risk of skin cancer recurrence or metastasis. Your dermatologist or medical care professional can help you decide on your best treatment option.
A skin biopsy is normally covered by Medicare, Medicaid, and insurance companies, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this usually covers your co-payment.
SURGICAL THERAPIES
(1) Electrodessication and Curettage Treatment for Squamous Cell Carcinoma
Electrodessication and Curettage are two of the most common ways to treat non-melanoma skin cancers like Squamous Cell Carcinoma. This is sometimes
abbreviated ED&C or EDC or EC or CE (electrodessication and curettage), F&C or FC (fulguration and curettage). Electrodessication is when the electrosurgery probe touches the skin cancer area, while fulguration is when the probe is allowed to spark over the treatment area.
This treatment consists of local anesthesia followed by “burning” the skin with an electrosurgery probe (i.e. electrodessication and/or fulguration), then scraping the skin cancer area with a curette. This electrosurgery-curettage technique is usually repeated two or three times to destroy the underlying skin cancer. It has a cure rate of 95% or higher for skin cancers that are low risk (i.e. less than 1.0 cm or 0.4 inches in size).
Treatment is usually covered by Medicare, Medicaid, and insurance carriers, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.


TREATMENT OF A NON-MELANOMA SKIN CANCER (Basal Cell Carcinoma or Squamous Cell Carcinoma with ELECTRODESSICATION AND CURETTAGE (EDC))
A Squamous Cell Carcinoma should be treated to prevent enlargement and spread (metastasis).
LEFT After the area is numbed up with local anesthesia, the area is cauterized (burned) with the probe of an electrosurgery device, as shown here.
RIGHT - The area is then curetted (scraped), then cauterized again for two or more times to remove any residual cancer.
Note that some dermatologists prefer to curette larger or deeper skin cancers first followed by electrodessication (burning).
Skin cancer is often treated with electrodessication (“burning” with the probe of an electrosurgery unit), followed by curettage. This is usually repeated 2–3 times.
(2) Excision of Squamous Cell Carcinoma
Your dermatologist or medical professional may cut out (i.e., excise) your skin cancer under local anesthesia using a scalpel. The excised skin cancer is sent to a pathologist for processing and examination under a microscope to be certain that the skin specimen margins are free of skin cancer. Some skin cancer excisions are large and may require a second surgery to cover the skin cancer treatment site with adjacent normal skin (a skin flap) or adjacent detached normal skin (a skin graft). Excision usually requires cutting around the skin cancer with a 0.4 cm (0.2 inches) to 1 cm (0.4 inches) margin. Excision has a 95% or higher cure rate for low-risk skin cancer (1 cm or 0.4 cm in size) but does not do as well with high-risk skin cancer (over 1 cm or 0.4 cm in size).
Excisional treatment is covered by Medicare, Medicaid, and insurance carriers, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.

Squamous Cell Carcinoma on the right lower neck
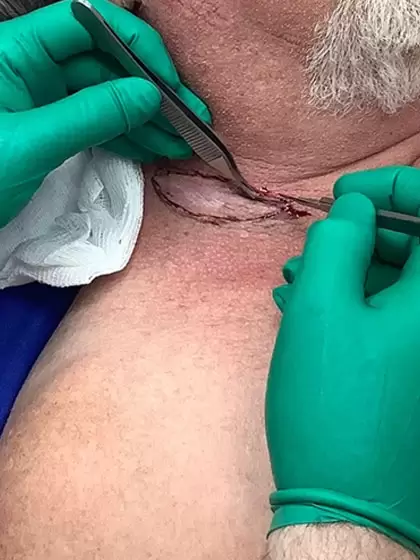
Excision of the skin cancer

Suturing of the skin cancer site
(3) Cryosurgery for Basal Cell Carcinoma
Cryosurgery treatment is occasionally used to treat skin cancer. Cryosurgery, itself, may cause scarring and occasionally disfigurement. Some dermatologists use cryosurgery for Superficial Basal Cell Carcinomas (BCC) and Squamous Cell Carcinomas (SCC) in elderly patients and in resistant BCCs and SCCs which have ill-defined borders or depth. Mohs surgery [see (5)] or Superficial Radiation Therapy (SRT) [see (6)] are usually preferred over cryosurgery.
This type of cryosurgery treatment consists of spraying liquid nitrogen in two freeze-thaw cycles of one minute each. The treated areas will become frozen and turn white. After two freeze-thaw cycles, the white color fades over several minutes. The treatment site then becomes red and swollen, and it may form a draining wound over several days or weeks. The area will take 4–6 weeks or longer to heal. For the best cosmetic result, gently cleanse the treatment site twice a day with mild soap and water, followed by the application of Vaseline or Aquaphor.
Cryosurgery for skin cancer is normally covered by Medicare, Medicaid, and insurance companies, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.

CRYOSURGERY UNIT
Cryosurgery is commonly used to treat pre-cancerous growths (Actinic Keratoses).
It is rarely used to treat non-melanoma skin cancer (e.g. Basal Cell Carcinoma and Squamous Cell Carcinoma).
(4) Laser Treatment for Squamous Cell Carcinoma in situ
A laser is sometimes used to treat Superficial Non-Melanoma Skin Cancer. Your dermatologist or medical professional uses a focused beam of light (laser) under local anesthesia to destroy superficial non-melanoma skin cancer (e.g., Squamous Cell Carcinoma or Basal Cell Carcinoma).
Medicare, Medicaid, and insurance carriers may cover laser treatment for skin cancer minus any deductible or co-payment. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.

Squamous Cell Carcinoma
in situ on the right lateral cheek

After treatment with a carbon dioxide (CO2 ) laser.
Note the redness and crusting of the treatment site.
(5) Mohs Surgery for Squamous Cell Carcinoma
Mohs surgery is named after Fredric E. Mohs (1910-2002), who pioneered this procedure. Mohs surgery is considered the “Gold Standard” for non-melanoma skin cancer treatment. It is generally performed on high-risk areas around the eyes, ears, nose, or mouth areas and for recurrent skin cancer. There is up to a 99% cure rate with Mohs surgery, which is superior to most other forms of skin cancer treatment. Superficial Radiation Therapy (SRT) also has a very high cure rate of 98–99%.
If you are referred to a Mohs surgeon, the Mohs surgeon will evaluate your skin cancer site. Your skin cancer will be removed in stages under local anesthesia, usually on the same day. A layer of skin is removed in each stage, and the tissue is processed and examined under a microscope at an on-site laboratory.
This is repeated until the skin cancer has been completely removed. During your office visit to a Mohs surgeon, you will have to wait between each stage for your skin specimen to be evaluated under a microscope. Plan for your visit to a Mohs surgeon to take several hours or longer.
You may also be required to stay longer after your Mohs surgery if there is a large surgical wound created by your Mohs surgery treatment. This wound may be allowed to heal naturally over 4–6 weeks. Alternatively, complex repair or a skin graft/skin flap are used to cover the Mohs surgery site.
Medicare, Medicaid, and insurance carriers generally pay for Mohs surgery minus any deductible or co-payment. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.

Squamous Cell Carcinoma on the left cheek

After Mohs treatment.
Note the skin cancer is much larger than expected.

After surgical repair of the Mohs defect with an advancement flap.
NON-SURGICAL TREATMENTS FOR SQUAMOUS CELL CARCINOMA
(6) SUPERFICIAL RADIATION THERAPY (SRT) FOR SQUAMOUS CELL CARCINOMA
Radiation therapy has been used to treat skin cancer since 1896. Treatment is based on Wilhelm Rontgen’s remarkable discovery of X-rays on November 8, 1895. Over the last century, radiation therapy has evolved. In the past 8 years, safe, reliable radiation machines have been developed that use tungsten (used in light bulbs) instead of radioactive materials to treat Basal Cell and Squamous Cell Carcinomas.

One of the first X-rays taken was on December 22, 1895 of the hand of Wilhelm Rontgen’s wife.
Within months, radiation was being used to treat skin cancer.
Sensus Healthcare™ is a pioneer in radiation therapy and manufactures the Sensus SRT 100™, 100+™, and Vision™ radiation machines for skin cancer treatment. SRT uses superficial radiation, which does not penetrate deeply into your skin. In contrast, the hospital radiation machines treat below-the-skin surfaces for breast cancer, colon cancer, prostate cancer, and other internal cancers. For this reason, superficial radiation therapy (SRT) has few side effects compared to hospital radiation machines.
Several companies have recently developed radiation machines for the treatment of non-melanoma skin cancer (i.e. Basal Cell Carcinoma and Squamous Cell Carcinoma.) A comparison of these different radiation machines is not available at this time.
The advantages of Superficial Radiation Therapy (SRT) are:
SRT therapy is usually not used on children. It is also not recommended for patients with rare skin cancer disorders, genetic disorders like xeroderma pigmentosum and albinism, or rare skin cancers that are resistant to radiation therapy. Mohs surgery [see (5)] is the preferred treatment in these cases.
Superficial Radiation Therapy (SRT) is covered by Medicare, Medicaid, and insurance carriers minus any deductible or co-payment. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.
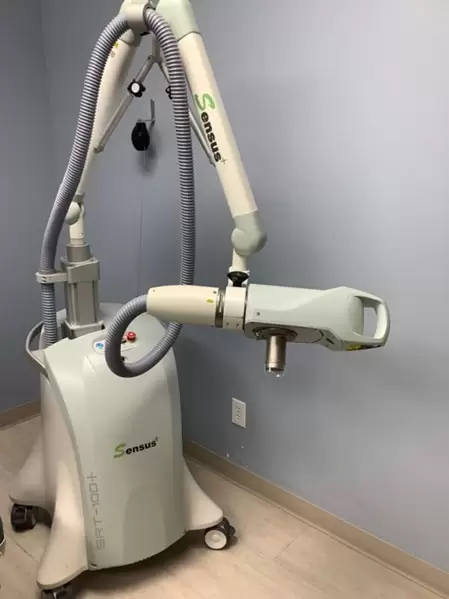
Sensus SRT 100+ Radiation machine
Superficial radiation machines are very safe. They produce radiation by using tungsten. This is the same element that is found in an electric light bulb.

Treatment for non-Melanoma Skin Cancer (e.g. Basal Cell and Squamous Cell Carcinomas) with Superficial Radiation Therapy (SRT).
(7) Chemical Treatment for Squamous Cell Carcinoma
Traditional Chemical Treatment is NOT recommended for an initial Squamous Cell Carcinoma except in unusual circumstances. Topical chemical creams, ointments, and solutions do not penetrate deeply enough into the skin
An anti-cancer cream or ointment of solution like 5-Fluorouracil 5% or Imiquimod 5% is sometimes used to treat sites that have already been treated for skin cancer. They are also sometimes used with elderly or non-compliant patients. One treatment regimen is to apply 5-Fluoruracil 5% cream twice a day for 6–8 weeks or longer, depending on the response to treatment. Alternatively, Imiquimod 5% cream is applied twice a day for 16 weeks or longer, depending on the response to treatment.
Medicare, Medicaid, and most insurance companies will cover your office visit for treatment of Actinic Keratoses and skin cancer minus any deductible or co-payment. If you have a second insurance policy (“secondary insurance”), this will usually pay for your co-payment. Your insurance company may not pay for or may delay payment for your anti-cancer cream, ointment, or gel. This problem can be avoided by sending your prescription directly to a specialty pharmacy through your doctor’s office.
TREATMENT FOR ADVANCED SQUAMOUS CELL CARCINOMA
Most Squamous Cell Carcinomas can be successfully treated if diagnosed early. Squamous Cell Carcinoma can invade underlying skin structures as well as spread (metastasize) to other areas of the body. There are a number of new drug therapies that may shrink or help control advanced Squamous Cell Carcinoma:
Cemiplimab-rwlc (Libtayo™ ) and Pembrolizumab (Keytruda™) which are administered intravenously. These drugs can be used before surgery to shrink an advanced Squamous or Basal Cell Carcinoma or after surgery to treat skin cancer that is resistant to surgery.
These treatments are covered by Medicare, Medicaid, and other insurance carriers, minus any deductible or co-payment required by your insurer. If you have a second insurance policy (“secondary insurance”), this will usually cover your co-payment.